An Austin Sleep Therapist Explains: The Science Behind Insomnia
Sleep and wakefulness are two processes that are constantly competing with one another. Only one can win at any given time, and you want the right one to win at the right time. If you have a sleep disorder like insomnia, you're finding yourself awake when you desperately want to be asleep.
For those seeking insomnia treatment in Austin, understanding the "why" behind your sleep disruption is the first step toward finding a solution. Two core biological processes have a massive impact on your sleep: Process S (your sleep drive) and Process C (your circadian rhythm). When one or both of these get out of sync, sleep problems begin.
The Two Key Players in Your Sleep
To get the deep, quality rest you need, it's crucial to understand the two systems that govern it.
Process S: Your Sleep Drive
You can think of your sleep drive (also called your sleep homeostat) as your body's appetite for sleep. It determines how much sleep you get and the quality of that sleep. The longer and more active your day is, the more sleep drive you build.
Imagine you're filling a balloon all day long. By bedtime, that balloon should be full enough to deflate slowly, carrying you through the entire night. If you haven't built enough pressure, you won't get to sleep or stay asleep. This is why going to bed earlier when you’ve slept poorly often backfires—the sleep drive simply isn't there yet. It has nothing to do with the clock; it’s only about how much "sleep pressure" has accumulated.
Process C: Your Circadian Rhythm
Your circadian rhythm is your internal 24-hour clock. Every cell in your body has one, and it dictates the timing of when you feel sleepy and when you feel alert. If you’ve ever had jet lag, you’ve felt your circadian rhythm trying to catch up to a new time zone—feeling sleepy, awake, and hungry at odd times.
This internal clock gets confused by erratic schedules. Wildly different bedtimes and wake times, inconsistent meal times, and irregular light exposure can make your body feel like it's flying coast to coast every day. Your circadian rhythm doesn't know if it's day or night, leading it to make poor judgment calls about when to promote sleep or wakefulness.
When these two processes work together, your sleep drive is high right as your circadian rhythm signals it's time for bed, creating the perfect window for sleep. My goal in insomnia treatment in Austin, TX, is to get these two powerful processes working in harmony again.
Here is a visual of these two processes working together. Insomnia treatment in Austin can address issues with either or both.
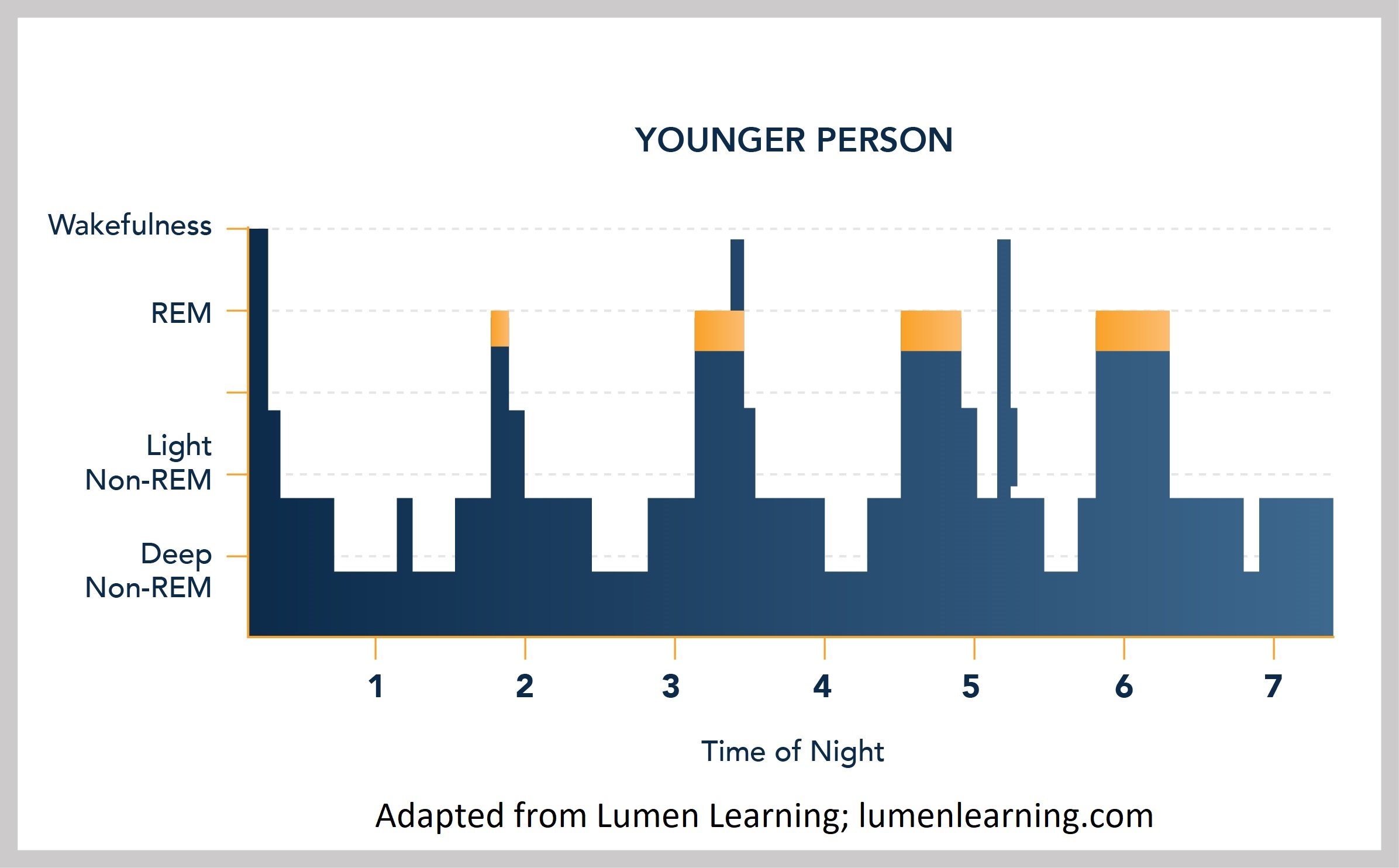
A Look at Your Sleep Architecture
Over the course of a night, your brain cycles through different stages of sleep. This is your "sleep architecture."
N1 (Stage 1): A very light stage of sleep, which you're in just as you doze off. You're easily awakened here.
N2 (Stage 2): A slightly deeper stage where your body continues to slow down. You spend most of your night—about 45-55%—in N2 sleep.
N3 (Stage 3): This is deep sleep, also known as slow-wave sleep. It's when your body does most of its physical repair. You are very difficult to wake during this stage. Most deep sleep occurs in the first half of the night.
REM (Rapid Eye Movement): This is a lighter stage of sleep where most dreaming occurs. It's crucial for emotional processing and memory consolidation. Most REM sleep happens in the second half of the night.
A healthy sleeper cycles through these stages multiple times. For those with insomnia, this architecture is often fragmented and disrupted.
Here is an idea of what someone’s sleep architecture might look like over the course of the night. Someone with insomnia will often have less deep sleep.
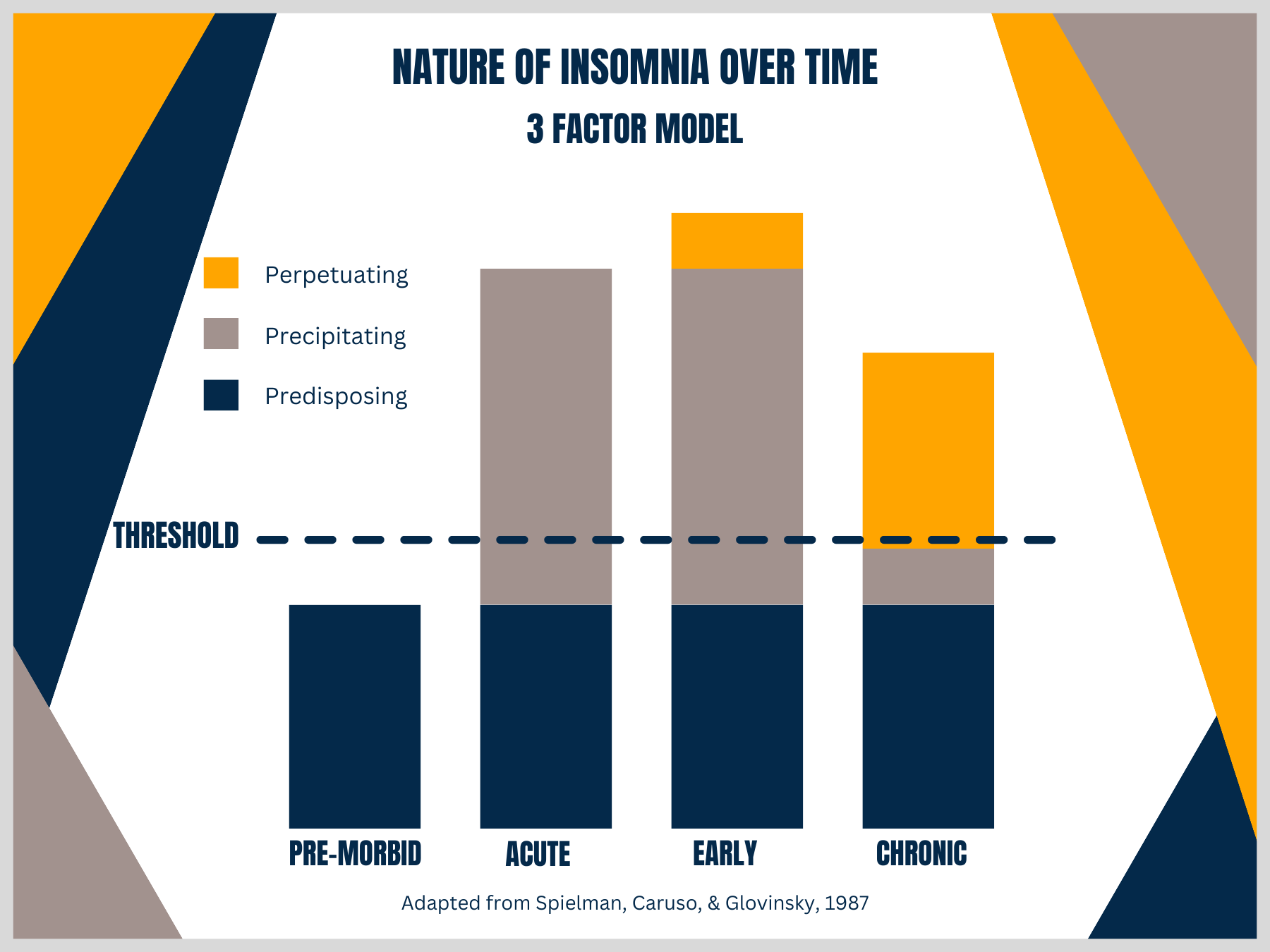
The Behavioral Model of Insomnia: How Sleep Problems Stick Around
Insomnia often begins as a temporary issue but can evolve into a chronic, learned habit. We look at this through a model of three factors.
The 3 "P's" of Insomnia
Predisposing Factors: These are the traits that might make you more vulnerable to developing insomnia. This can include a tendency toward anxiety, a high level of conscientiousness, a family history of insomnia, or a history of trauma. These factors don't cause insomnia, but they push you closer to the threshold.
Precipitating Factors: This is the event or trigger that kicks off the sleep problem. It's often a major life transition (even a positive one!) like a new job, a divorce, having a baby, or moving. Medical issues like chronic pain, GI issues, or mood disorders can also be precipitating factors.
Perpetuating Factors: This is the most important area we target in treatment. These are the things you start doing in an attempt to fix your sleep that actually make it worse and keep the insomnia going, long after the initial trigger is gone. Your focus shifts from "I can't sleep because of X" to simply "I just can't sleep."
This is a well-known model for understanding insomnia.
The Three Paths to Chronic Insomnia
The perpetuating factors that lock insomnia in place typically fall into one of three categories. A good sleep therapist in Austin will help you identify which of these paths you've gone down.
Path 1: Disrupted Sleep Drive
This path involves behaviors that weaken your sleep drive, leaving you without enough "sleep pressure" to fall and stay asleep at night.
Spending excessive time in bed: This is the single biggest factor for many people. If you spend 10 hours in bed but only sleep for 6, your sleep becomes shallow and fragmented.
Napping incorrectly: Naps spend your sleep drive. If you don't have enough in the bank, a nap can steal from your nighttime sleep.
Staying in bed while awake: Lying in bed for more than 30 minutes after waking in the morning or trying to "catch up" on sleep just teaches your brain that the bed is a place for frustrated wakefulness.
Path 2: Circadian Rhythm Disruption
This path is about an inconsistent schedule that confuses your internal clock.
Variable wake-up times: A rise time that varies by more than an hour from day to day is a primary culprit. It gives your body a form of social jet lag without ever leaving home.
Ignoring your chronotype: A natural "night owl" forcing themselves onto an "early bird" schedule (or vice-versa) is fighting against their own biology. This mismatch often leads to lying in bed awake for hours because you're trying to sleep before your body is ready.
Path 3: The Arousal Factor
This is when anxiety and unhelpful thinking habits come in and override your body's natural sleep systems.
Sleep Effort: This is the act of trying to sleep. Good sleepers don't try; they just sleep. Trying to force or control sleep creates performance anxiety, which is the enemy of rest. If you're meditating, relaxing, or just lying there in order to sleep, you're exerting sleep effort.
Worrying in Bed: Using your bed as a place to worry—about sleep itself, your health, finances, or family—trains your brain to associate the bedroom with stress and alertness.
Conditioned Arousal: This is the frustrating phenomenon where you feel sleepy on the couch, but the moment your head hits the pillow, a switch flips and you're wide awake. Your brain has learned to associate the bed with being alert and anxious, not with sleep.
If these patterns sound familiar, know that you're not alone. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective, evidence-based approach that directly targets these perpetuating factors. If you are looking for effective insomnia treatment in Austin TX, reach out today to schedule a consultation.